Last partial update: July 2017 - Please read disclaimer before proceeding.
Assessing heart attack risk level
Thankfully, not everyone is going to die from vascular disease (blockage of arteries). Indeed, illness due to to cardiovascular disease has reduced in Australia over the past 40 years by about a third; mainly due to reduced smoking levels, improvements in diet and better medical care. (A much better result could have been attained if obesity, lack of exercise and diabetes had not worsened during this period!)
However, cardiovascular disease remains the leading cause of death in Australia for both men and women and it is important for doctors and patients to try and find out who is most likely to suffer from these diseases so that they can be specially targeted for treatment.
Only about 40% of deaths from heart attacks occur in people who already have illness from cardiovascular disease (i.e. a previous heart attachk, angina, stroke, TIA or peropheral vascular disease.) This means that 60% of deaths occur in people who have had no symptoms of cardiovascular disease and most are unaware they have underlying disease. Determining who these people are and treating them before sypmtoms occur is the foundation of cardiovascular disease prevention.
Research has established that about 90 per cent of vascular disease is due to known cardiovascular disease risk factors and, with this degree of certainty, overall risk factor assessment has established itself as the fundamental method for determining a person’s likelihood of suffering from the main vascular diseases; heart attacks and strokes. Most of the research on risk factors has been done for assessing heart attack risk and thus this section focuses on this particular disease.
HOWEVER: Trying to predict who will have a heart attack and who won't is still difficult. This is because at least half of the heart attacks that occur do so in people who are not at high risk. Thus, it is important for everyone to try to lead healthy lives so that their risk is reduced.
Risk factors for heart attacks
The numerous factors that increase a person’s risk of vascular disease are mentioned below. Those that can be modified by lifestyle change or medication are specially marked with an asterix(*).
Diseases already present that increase cardiovascular disease risk
(The effect of most of these diseases can be reduced with appropriate treatment / lifestyle modification)
- Known cardiovascular disease (heart attack, angina, stroke, transient ischaemic attack (mini-stroke), artery disease in the legs, aortic aneurysm.
- Evidence of atrial fibrillation (an abnormal heart rhythm)
- Diabetes
- Impaired kidney function (especially where there is significant protein in the urine (found by a simple ‘stick-test’ of urine))
- Polycystic ovarian disease
Biological and lifestyle risk factors that can be modified
- High blood pressure (A major factor in causing strokes as well as heart attacks.)
- Abnormal blood fats (lipids) (especially elevated total cholesterol and LDL cholesterol)
- Smoking
- Physical inactivity (This is the greatst risk factor for women over 30 years of age.)
- Abdominal obesity. (This is best measured by waist size with optimal levels being less than 80cm for women and 94cm for men. (See section on obesity). Waist circumference is a better indicator of cardiovascular risk than body mass index (BMI)).
- Poor nutrition (especially excess dietary saturated fat)
- Excessive alcohol consumption (causes increased blood pressure)
- Depression
Biological and lifestyle risk factors that cannot be modified
- Age greater than 50
- Strong family history of heart disease (First degree relative (a parent or sibling) affected before 60 years of age)
- Lower socio-economic status
- Male gender. This incidence of developing cardiovascular diseae is the same for men as it is in women. (In both men and women aged 55 years, about two thirds will go on to have some form of significant cardiovascular disease. The reason male gender is a risk factor for developing cardiovascular disease is that cardiovasuar disease occurs about 10 years earlier in men. Women do have a slightly higher incidence of developing stroke than men. (Interestingly, the likelihood of a woman dying of a heart attack is five times that of dying of breast cancer.)
- Higher risk ethnic groups (Indigenous Australians, Torres Strait Islanders, Maoris, Pacific Islanders, people from the Indian sub-continent)
- Social isolation
Incidence of some modifiable risk factors in adult Australians |
||
Risk Factor for vascular disease |
Incidence in adults |
|
Males |
Females |
|
Diabetes |
8% |
7% |
High cholesterol |
51% |
51% |
Inadequate physical activity |
34% |
35% |
Smoking |
27% |
20% |
High blood pressure |
31% |
28% |
Overweight (BMI > 25) |
68% |
53% |
Risk factor incidence
The large mortality associated with cardiovascular disease is not surprising when the prevalence of cardiovascular risk factors is examined. About 80 per cent of the adult population has at least one major risk factor for coronary artery disease and 10 per cent have at least three major risk factors.
Some of the most important risk factors are not modifiable, including age, male gender and a family history of cardiovascular disease. However, many important factors that occur commonly in the community are modifiable. These are detailed in the table above.
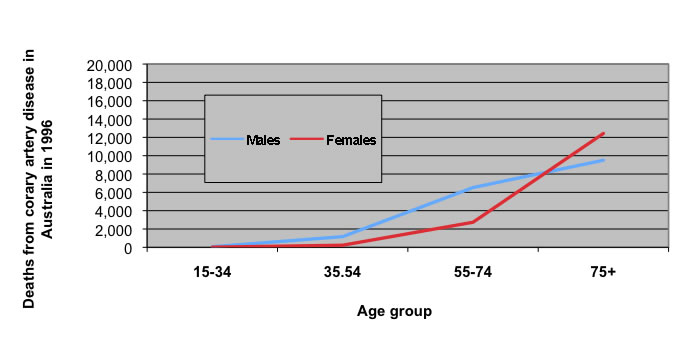
The figure below, which shows the relationship between age and deaths from cardiovascular disease, indicates how important a risk factor increasing age is in both sexes. This fact means that everyone needs to take steps to reduce their risk factors.
Age related death rates from coronary artery disease in Australia in 1996
|
(Back to top)
Overall cardiovascular disease (heart attack) risk
Currently, when doctors in Australia assess cardiovascular disease risk in patients, they divide them into three risk groups depending on the likelihood of them suffering a ‘cardiovascular event’ in the next 5 years. A cardiovascular event includes the following; death from vascular disease, having a heart attack or starting to suffer from angina (heart pain), having a stroke or a transient ischaemic attack (a mini-stroke where the stroke-like symptoms disappear quickly). (In the USA the definition of a cardiovascular event is narrower and they express the risk over a period of 10 years. It is thought that the USA definition overestimates cardiovascular disease risk.)
High risk: This implies that the person has a 15% or greater risk of having a cardiovascular event over the next 5 years
Moderate risk: This implies that the person has a 10% to 15% risk of having a cardiovascular event over the next 5 years.
Low risk: This implies that the person has a less than 10% risk of having a cardiovascular event over the next 5 years.
At what age should cardiovascular disease risk level assessment start and how often should it be reassessed
Starting age: For most adults, 45 years is the age at which cardiovascular disease risk should start to be assessed. People at high risk should start earlier. This group includes Aboriginal people and Torres Strait Islanders who should start at age 35 years; and it also includes people with diseases that put them at high risk. (See Task 1 below.)
Frequency of assessment: The frequency of reassessment depends on the risk level.
- Low risk: reassess every 2 years
- Moderate risk: reassess every 6 to 12 months
- High risk: reassessment depends on severity, but it should occur at least every 3 to 6 months
Calculating a person’s cardiovascular disease risk level
The process of determining which risk group a person is in is done in two parts as follows.
Task 1: Determine if you are in a high-risk category.
There are six groups of people who are automatically deemed as being at high risk. These six groups are:
- People who have already had a heart attack or suffered from angina (chest) pain.
- People who already suffer from other vascular disease. This includes those who have had any of the following.
- A stroke or a transient ischaemic attack,
- Other vascular disease such as a blockage in the arteries supplying the legs (peripheral vascular disease) or an aortic aneurysm.
- An abnormal ultrasound investigation of an artery
- People with diabetes who:
- are over the age of 60 years or
- have kidney disease (from their diabetes) that causes significant loss of protein in the urine (i.e. albuminuria > 20 micrograms/min)
- People with chronic moderate to severe kidney disease resulting in:
- an eGFR level of less than 45 (The eGFR is a measurement of kidney function. See section on kidney disease.)
- significant chronic protein loss from the kidney into their urine.
- receiving a kidney transplant.
- People with total cholesterol greater than 7.5mmol/L or familial hypercholesterolaemia. (This is an inherited disease that causes very high blood cholesterol levels. Those with familial combined hyperlipidaemia are also at high risk.)
- Very high blood pressure: Systolic blood pressure (upper reading) > 180mmHg or diastolic blood pressure (lower reading) > 110mmHg
Task 2: Use the National Heart Foundation risk calculator to determine overall risk level.
If the person is not included in one of the six groups above, then a risk calculator is used to ‘add’ risk factors together to give an overall ‘risk level’.
The ‘Australianabsolute cardiovascular disease risk calculator’ is one of several calculators available for assessing a person’s overall cardiovascular risk and is the one that is at present recommended by the National Heart Foundation. (To access thie calculator click on the 'purple link' above or type into google 'Australian absolute cardiovascular disease risk calculator').
As discussed above, the person’s risk level is expressed as the chance that person has of suffering a ‘cardiovascular event’ in the next 5 years.
None of the risk calculators are perfect and there are some circumstances where this calculator is less accurate, including the following.
- In younger people. The risk calendar is not validated for use in people uder the age of 30 years.
- In the elder people (people over 75 years of age) For people over the aged 75yrs and over, use 74yrs as the age when using the calculator.
- When the person has very high blood pressure and / or cholesterol levels
- In Indigenous people, where it underestimates risk. As stated before, most Indigenous Australians are automatically categorised as being at high risk.
The risk factors used by the calculator are:
- The person's age
- The person's sex
- Systolic (uppper level) blood pressure. (In people on blood pressuse medication, the reading used should be level present before treatment was commenced.
- Whether the person currently smokes
- Whether the person has diabetes
- The person's total cholesterol level divided by their HDL cholesterol level (In people on cholesterol lowering medication, the readings used should be levels present before treatment was commenced.
- Whether the person has an enlargement of the left ventrical part of the heart (Most people will be unaware of whether they have this and it can be left as 'unknown'.)
Risk factors not considered by the calculator: A reason for an upgrade in their calculated risk level?
The National Heart Foundation cardiovascular disease risk calculator does not take into account some important risk factors, including the following.
- Significant family history
- The presence of mild kidney disease
- Polycystic ovarian syndrome (See section on other cardiovascular disease risk factors.)
- Depression / socioeconomic hardship
- People with atrial fibrillation: People with the abnormal heart rhythm called atrial fibrillation are at abnormal risk of having a cardiovascular event and the calculator can significantly underestimate the risk in these people.
- Significant obesity* (Waist size is much more important than actual weight.)
- inadequate physical activity*
*Both physical activity and obesity affect blood pressure, cholesterol levels and diabetes and thus their influence is included in the risk assessment calculation; it's just done indirectly.
Consideration needs to be given regarding upgrading the calculated risk level in the people with the above risk factors. This will vary according to individual circumstances and needs to be discussed with a medical practitioner. There are no set rules and it is important to remember that many heart attacks occur in people who are not at high risk.
In these cases or where risk level is borderline (low/medium or medium/high), some practitioners use coronary artery calcium assessment, done using a CT scanner. The level of calcium in coronary arteries has been shown to reflect the egree of disease in the artery. A person with a lower risk level but a strong family history of ischaemic heart disease can choose to have this test done to see whether their level of calcium is higher than would be expected from their calculated risk level. If it is this may change the person's management. This investigation is discussed further below.
Younger adults and the calculator
It is important to emphasise that the calculator is principally designed to identify people at significant risk who require medication to reduce that risk. Many younger people who have significant risk factors will be deemed to be at low risk because of their age. Lifestyle factors such as smoking, obesity and inadequate physical activity still need to be addressed in these younger people as this may help prevent them becominh high risk individuals as they age and thus may prevent or delay their need for mediation later in life to reduce risk.
Accessing the Calculator
The National Heart Foundation has an simple on-line calculator at: www.cvdcheck.org.au
Please remember that the risk calculator can only give an approximate idea of your overall risk as there are influential factors, such as physical activity level, family history and weight, that are not used in calculating overall risk. Thus, the risk result is no guarantee one-way or the other. To ensure that your result is properly interpreted, it is best to do your calculation with your doctor. It is also VITAL that you discuss your calculator result with your doctor before making decisions regarding lifestyle change and other treatment.
|
Most people who suffer from heart attacks have several mildly elevated risk factors While people who are at high risk of cardiovascular disease have a higher rate of developing the disease, it is vital to realise that the majority of heart attacks (and deaths from heart attacks) actually occur in people with several risk factors that are slightly raised who have a ‘low-ish’ overall risk (i.e. a 5-year risk of less than 10 to 15 per cent). This is because there are a lot more people in the lower risk groups. (Most heart attacks occur in people with total cholesterols of around 5.0 to 5.5mmol/L, not 8.0mmol/L.) Doctors are good at seeing the ‘red light’ of a very high cholesterol or a very high blood pressure and are good at aggressively treating these conditions. However, in a busy surgery, the person with several mild abnormalities is often missed or under-treated. People with several mild risk factors need to make sure their risk factors are well looked after. It is also true that several mild risk factors often actually places a person at higher risk than another person with one very high risk factor, such as a cholesterol of 8.0mmol/L. Age is a very important risk factor – ‘When I’m sixty-four’ Increasing age is the most important risk factor in older people (over 65 years of age) and is the one risk factor everyone does not wish to avoid, for obvious reasons!! Its effect will be less if other risk factors are minimized and this is best done by reducing other risk factors early. Making changes at 64 years of age may be too late. |
Patient management depends on level of risk
Treating 'low risk' patients
Cardiovascular disease is very common and everyone needs to think about reducing their risk by modifying their lifestyle. This is especially the case when the person has risk factors but is classified as low risk because of their relatively young age.
As well as reducing cardiovascular risk, increasing fitness levels and losing weight have other health benefits including cancer reduction and improved mental health.
Treating 'moderate risk' patients
People at moderate risk of cardiovascular disease need to be as aggressive as possible in reducing their lifestyle cardiovascular risk factors.
They also need to treat aggressively (usually including medication) any ‘disease’ risk factors aggressively, including high blood pressure, high blood lipids (cholesterol and/or triglycerides) and heart failure.
Treating 'high risk' patients
People at high risk of having a cardiovascular ‘event’ need to have all possible risks treated aggressively. This includes the following.
- Lifestyle modification. It is unfortunate that some people feel that taking medications to lower blood pressure, cholesterol etc is an adequate substitute for aggressively adopting a healthy lifestyle. This is not the case. The pairing of high risk and an unhealthy lifestyle is often a fatal combination, irrespective of which medications are being consumed!!!!!
- Treating with medication conditions that increase risk. These include diabetes, kidney disease, high blood pressure, high blood lipids (cholesterol and/or triglycerides), heart failure and heart arrhythmias.
- Add preventative medication.
It has been shown that lowering blood pressure and cholesterol can be a significant benefit to high-risk patients even when their pre-treatment levels are in the acceptable range for normal risk people. The optimum level for blood pressure is about 115mmHg* for the upper (systolic) reading and for total cholesterol is about 3.8mmol/L and any reduction towards these levels is likely to be of benefit in reducing cardiovascular disease risk and is warranted in people at high risk of vascular disease.
Unfortunately not all people at high risk qualify for subsidised medication to lower their cholesterol / blood pressure.
Also, some people at high risk will benefit from taking anticoagulants, such as aspirin, to reduce the chance of clotting in their arteries and thus help prevent heart attacks. It needs to be emphasised that these medications can be dangerous and the benefits outweigh the risks only in those at high risk of cardiovascular disease. It should only be used when prescribed by a doctor.
Unfortunately up to 50 per cent of patients at high risk of cardiovascular disease are not taking optimum medication.
(*Not all people can reach this blood pressure and for some, especially the elderly, it can be dangerous as it may make them feel dizzy and more likely to fall and injure themselves.)
Summary of recommended treatment according to risk level |
|
Risk level |
Advice |
Low risk |
Monitor Minimise lifestyle risk factors as appropriate. |
Moderate risk |
Treat individual risk factors / diseases Lifestyle modification |
High risk (This includes moderate risk people who have been upgraded to high risk.) |
Add medication to reduce cholesterol, blood pressure and blood clotting as appropriate. Treat individual risk factors. Lifestyle modification. |
(Back to top)
A ‘program’ for heart attack prevention
1. Reduce risk level by lifestyle modification
As cardiovascular disease is very common and successfully predicting who will suffer from it is not perfect, all adults should consider minimising their modifiable risk factors, especially if they also have non-modifiable risk factors such as a family history of heart disease. These measures include the following.
- Improving lifestyle risk factors
- Refrain from smoking.
- Strive to achieve a healthy waist measurement. (A waist measurement of less than 94cm in men and 80cm in women)
- Undertake adequate physical activity (See section on Physical inactivity.)
- Keep to a ‘healthy fat’ diet. (For most Australian diets, this means reducing both saturated fat and total fat intake.) Consuming seven servings of fruit and vegetables each day is also important.
How actively people need to pursue these measures will depend on their overall risk level. However, please remember that doctors still do not know all the risk factors for vascular disease and it is thus a wise policy to make sure the known ones are minimised.
- Optimise medical treatment of existing diseases that increase risk including:
- Diabetes
- High blood pressure
- Kidney disease
- Heart failure
2. Determine level of risk (See previous section)
People 45 years of age or over should determine their overall risk level for cardiovascular disease as described above. (This may need to be done from 35 years of age in people who have enough known risk factors to put them at significant risk. See list above.)
People will need to talk to their doctor about the health information they require to use the risk calculator. This information includes:
- Blood total cholesterol and HDL cholesterol levels (This is usually initially measured at 45 years, although initial cholesterol checks may need to be done earlier when risk is increased due to other factors such as family history of heart disease, high cholesterol, diabetes, kidney disease etc)
- Blood pressure measurement (A reading taken within the last year.)
- Fasting blood sugar test (This test is usually first done at age 55, although initialblood glucose checks may need to be done earlier in people who are at increased risk of developing diabetes. (See separate Diabetes section.)
3. All people need to discuss their risk level with their doctor.
4. Decide (with a doctor) whether medication is needed to reduce overall cardiovascular disease risk level.
This may include:
- Cholesterol lowering treatment. (This is the most commonly used medication to lower risk. Every 1.0mmol/L reduction in LDL cholesterol reduces the risk of a major cardiovascular event by 25%.)
- Medications to treat risk factors, such as medications for diabetes and hypertension.
- Medication to reduce blood clotting. Aspirin and other anti-clotting medications are helpful in preventing vascular disease in people at high risk. People at lower risk gain no overall benefit due to the side effects of the medication. (Long-term aspirin use can have very serious side effects and should ONLY BE USED when recommended by the person’s doctor.)
Medication and the prevention of cardiovascular disease in people who already have it (secondary prevention):
All people with existing cardiovascular disease (i.e. those who have had a heart attack or angina or a stroke etc) will benefit significantly from a blood pressure loweriong medication, a statin to lower blood cholesterol and an anti-platelet (anti-clotting) medication. Given together, these three medications can produce a reduction in the rate of cardiovascular events over the next 5 years of about 50%. This is a huge benefit and all prople with existing cardiovascular disease should be on all three medications unless they are unable to take them.
5. Regularly review risk level and treatment with a doctor
People need to remember that their risk of developing cardiovascular disease will change with time. It is therefore important to review risk regularly with a doctor. (Regular check ups, which should occur at least every 2 years, are a good opportunity.)
6. Get The Heart Attack Action Plan: A resource provided by the National Heart Foundation
Chest pain / heart attack action plans are available for download (or order forms) from the following web site:
http://www.heartattackfacts.org.au/action_plans/HeartAttackActionPlan-english.pdf
Modifying risk factors – how much does it help?
Lifestyle
Many studies have shown that reducing major risk factors does make a huge difference in preventing vascular disease. There are several lifestyle factors that have shown benefit including:
- Quitting smoking: (CVD risk reduces gradually after quitting and reaches approximately that of a non-smoker after 10 years)
- Maintaining a healthy body weight; Reducing weight in overweight people reduces cardiovascular disease throufgh causing a reduction in blood pressure, blood cholesterol levels and risk of diabetes.
- Partaking in adequate physical activity: Adequate physical activity reduces both cardiovascular disease and other cardiovascular disease risk factors such as diabetes and obesity and has many other health benefits. Adequate exercise for a healthy person can achieved by doing
- 150 to 300 minutes of moderately vigourous exercise per week or
- 75 to 150 minutes of vigorous exercise per week.
- Refraining from excessive alcohol intake: (less than 20g (or two standard drinks) per day)
- Consuming a healthy diet: There is much debate about the extent to which a healthy diet can influence CVD risk. Here are a few useful facts.
- Consuming a healthy balanced diet (similar to the Mediterranean type diet) helps reduce cardiovascular disease: There is good evidence that an improvement in diet has been an important contributor to the reduction in cardiovascular disease that has occurred over the past 40 years, with the best evidence of benefit being for a Mediterranean type diet. It is likely that multiple eements of this type of diet cause this beneficial effect ; not just a change in one factor, such as a change in the type of fat consumed.The National Health and Medical Research Council has created dietary guidlenes aimed at optimisng health generally called the Australian Dietary Guideines (2013) and these can be accessed via the following web site link. Australian Dietary Guideines (2013)
- Reducing dietary saturated and trans fats alone provides only a minor benefit: Reducing saturated fat does provide a moderate reduction in cardiovascular events and thus is still a dietary recommendation. However, alone it has not been shown to reduce deaths from cardiovascular disease or deaths generally.
- Reducing salt intake to below 6g per day helps reduce cardiovascular disease by reducing blood pressure.
Cholesterol
A reduction in cholesterol of 1.0mmol/L is generally considered to give a 25% reduction in the incidence of major cardiovascular events. This is irrespective of whether it is achieved through dietary change or medication. Similar benefits are gained by reducing blood pressure.
Family history – A risk factor that can’t be changed (Also see separate section on this topic.)
Many people inherit an increased risk of vascular disease. This is defined as having a first-degree relative (parent or sibling) who developed coronary artery disease (angina or heart attack) before the age of 60 years. A family history of coronary artery disease is an important risk factor and people who have such a history should take all measures possible to reduce any other risk factors they have.
It is also important to look for the cause of the relative’s coronary artery disease. If the relative had risk factors that can be prevented and the person does not suffer from these, such as smoking, high blood pressure, obesity or lack of exercise, then the family history may be less significant. If diabetes or high cholesterol were problems, then the person should be regularly tested for these conditions as they are to some extent inherited.
If the relative that developed coronary artery disease did not have any obvious risk factors and the family history is relatively strong, then consideration should be given to testing for a raised homocysteine level in the blood as this can be associated with increased vascular disease and is usually an inherited condition. Homocysteine is dealt with in the section on ‘Other cardiovascular disease risk factors’.
Further information about risk factors and reducing their incidence is presented in the following chapters and in other sections of this website (as detailed below)
- High cholesterol
- Hypertension (high blood pressure)
- Smoking cessation (See chapter on lung cancer.)
- Obesity (See separate section on obesity.)
- Physical inactivity (See separate section on physical inactivity.)
- Kidney disease (See final chapter in this section and chapter on kidney disease.)
- How to achieve lifestyle change
- Diabetes
Treatment target levels for people at high risk of heart attack
Treatment target levelsfor people at high risk of cardiovascular disease are detailed in the table below. These target blood pressure and lipid levels may not be able to be achieved in some people, either because the required doses of medications can not be tolerated or because maximum doses do not achieve the target levels.
Target levels for risk factors in people who have had a heart attack |
|
Risk factor |
Target level |
Systolic blood pressure (the higher reading) |
130mmHg (Benefit occurs to levels as low as 115mmHg) |
Diastolic blood pressure (the lower reading) |
85mmHg |
Smoking |
Nil |
Weight |
Waist circumference in males: 94cm Waist circumference in females: 80cm BMI of 20 to 25 |
Physical activity |
20 to 30 minutes per day of moderate activity |
Total cholesterol |
Less than 4.0mmol/L |
LDL cholesterol |
Less than 2.0mmol/L |
HDL cholesterol |
Greater than 1.0mmol/L |
Triglycerides |
Less than 1.5mmol/L |
Other methods of assessing cardiovascular disease riskC reactive protein measurement
Detection of calcium in arteries by electron beam computed tomography (a high resolution CT scan):
Assessing vascular disease in other arteries in the bodyFinding artery disease in other parts of the body is a good indicator that artery disease exists in the coronary arteries (the arteries supplying the heart).
|
Further Information
British Hypertension Society Risk Calculator
This is a calculator that people can actively use on their computer. It is best done with a doctor as it requires medical information that the person may not have available. It is located at:
http://bhsoc.org//index.php?cID=269